According to Harvard Health Blog, recent studies indicate that 50-80% of patients recovered from COVID-19 continue to have at least one adverse symptom three months after the onset, even if the patient no longer tests positive for the virus. This emerging condition has been described using a variety of terms including: “Post-Covid-19 Syndrome”, “Long COVID”, “Post-Acute Sequelae of SARS-COV2 infection (PASC)”, and “Long-Haulers”. As healthcare providers to the most vulnerable population, it is our duty to monitor the evolving evidence in this area and adapt for timely identification and intervention of needs.
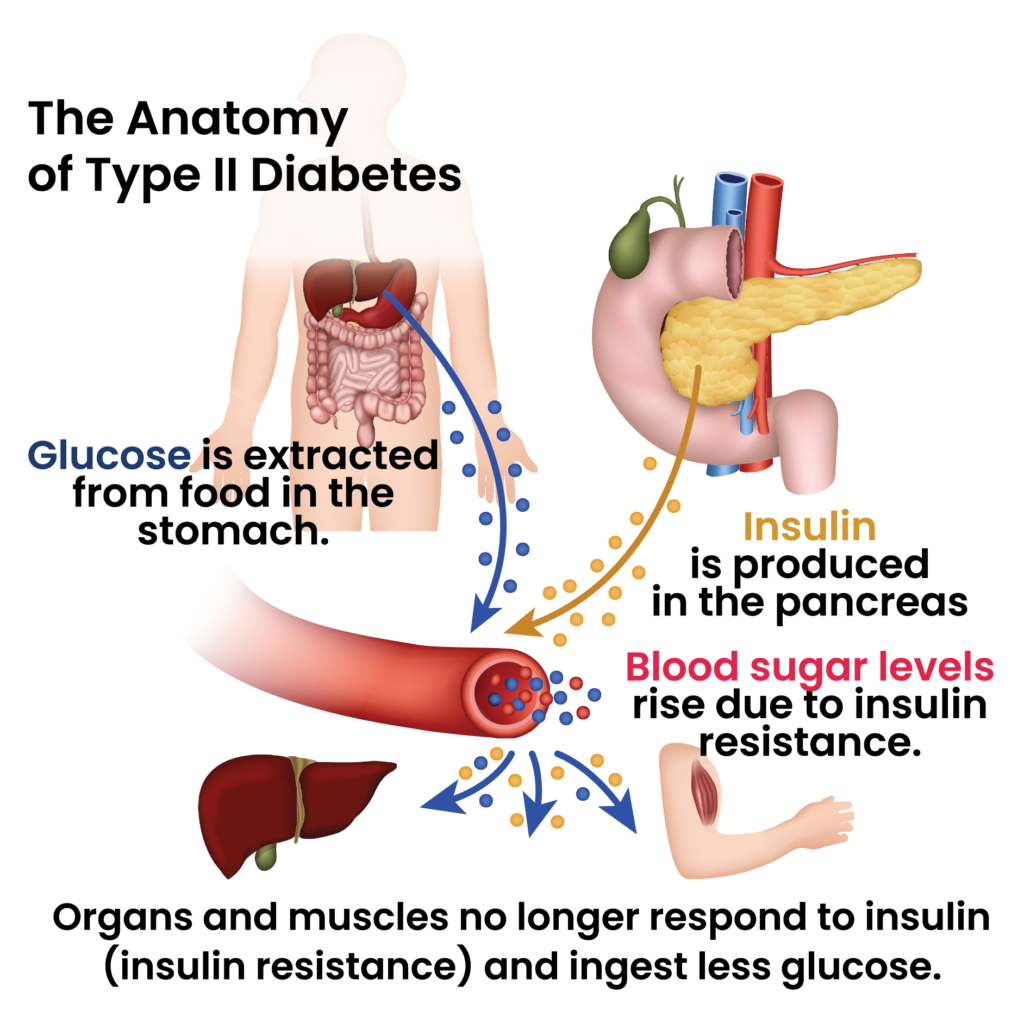
Though what predisposes an individual to developing “Long COVID” is still unknown, a number of those with even mild symptoms have continued to experience lingering effects. Some of the troublesome symptoms that have been observed with “Long COVID” include many of the same musculoskeletal, cardiopulmonary, oral/respiratory, neurological, and psychological dysfunctions that are seen with active COVID-19. Furthermore, it has been noted that some individuals recovering from COVID-19 develop new conditions or complications of pre-existing conditions as a result of the illness.
Rehabilitation’s distinct role in COVID recovery and “Long COVID” is clear. Therapy can intervene to assist “Long Hauler” patients by maximizing their participation and performance in daily function with the use of the following:
- Referral to the IDT when changes in clinical presentation emerge
- Patient-specific musculoskeletal and neurological re-training
- Individualized cardiopulmonary programming
- Dysphagia analysis and treatment
- Compensatory strategies to assist with cognitive re-training
- Environmental modifications to facilitate increased participation and decreased risk of injury
- Trauma-informed approaches to care when addressing the psychological effects of prolonged isolation
- Patient and caregiver training on adaptive techniques and equipment
- Patient education to promote health literacy
Reliant is actively engaged with the therapists in the field by developing resources such as Reliant’s Post COVID Clinical Considerations in order to equip the care team to positively impact patients and residents. Evidence continues to emerge, but the tools and knowledge do exist to address the physical, cognitive, and psychosocial needs that COVID-19 has introduced. Whether newly diagnosed as COVID positive, challenged by long-term effects of “Long COVID”, or facing an entirely new condition as a result of COVID-19, a patient or resident will never feel alone as they can rest assured that we’re with them for the long haul.
References:
Anthony Komaroff, MD. “The Tragedy of Long COVID.” Harvard Health Blog, 1 Mar. 2021, www.health.harvard.edu/blog/the-tragedy-of-the-post-covid-long-haulers-2020101521173.
AOTA. “Research: Occupational Therapy and Physical Therapy Provide Significant Rehabilitative Value in Post-Acute Care.” American Occupational Therapy Association, 5 Apr. 2021, www.aota.org/Advocacy-Policy/Federal-Reg-Affairs/Therapy-Outcomes-Post-Acute-Settings.aspx.
Cutter, Matthew. “COVID Long-Haulers: An End in Sight?” ASHAWire, 5 Mar. 2021, leader.pubs.asha.org/do/10.1044/leader.FTR1.26032021.42/full/.
Royal College of Occupational Therapists. “A Quick Guide for Occupational Therapists: Rehabilitation for People Recovering from COVID-19.” Rcot.co.uk, Apr. 2020, www.rcot.co.uk/files/guidance-quick-guide-occupational-therapists-rehabilitation-people-recovering-covid-19-2020.
WHO. “COVID-19 Clinical Management: Living Guidance.” World Health Organization, World Health Organization, 25 Jan. 2021, www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1.