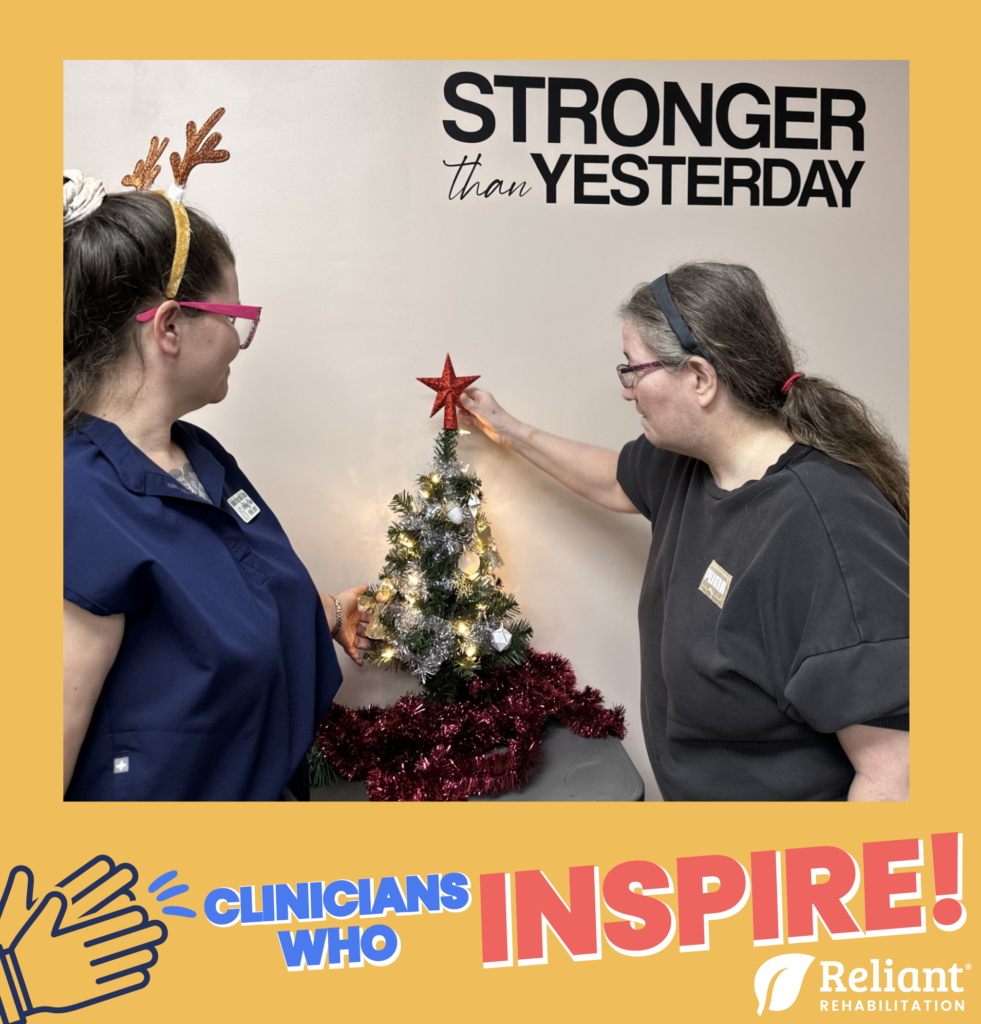
This month’s Clinician Who Inspires is Abby Fore, Champion Level I Therapist, PTA and DOR at The Blossoms at Prescott Rehab & Nursing Center. During the interview with Abby, it was clear that the rehab gym at Prescott is truly jingling with holiday delight.
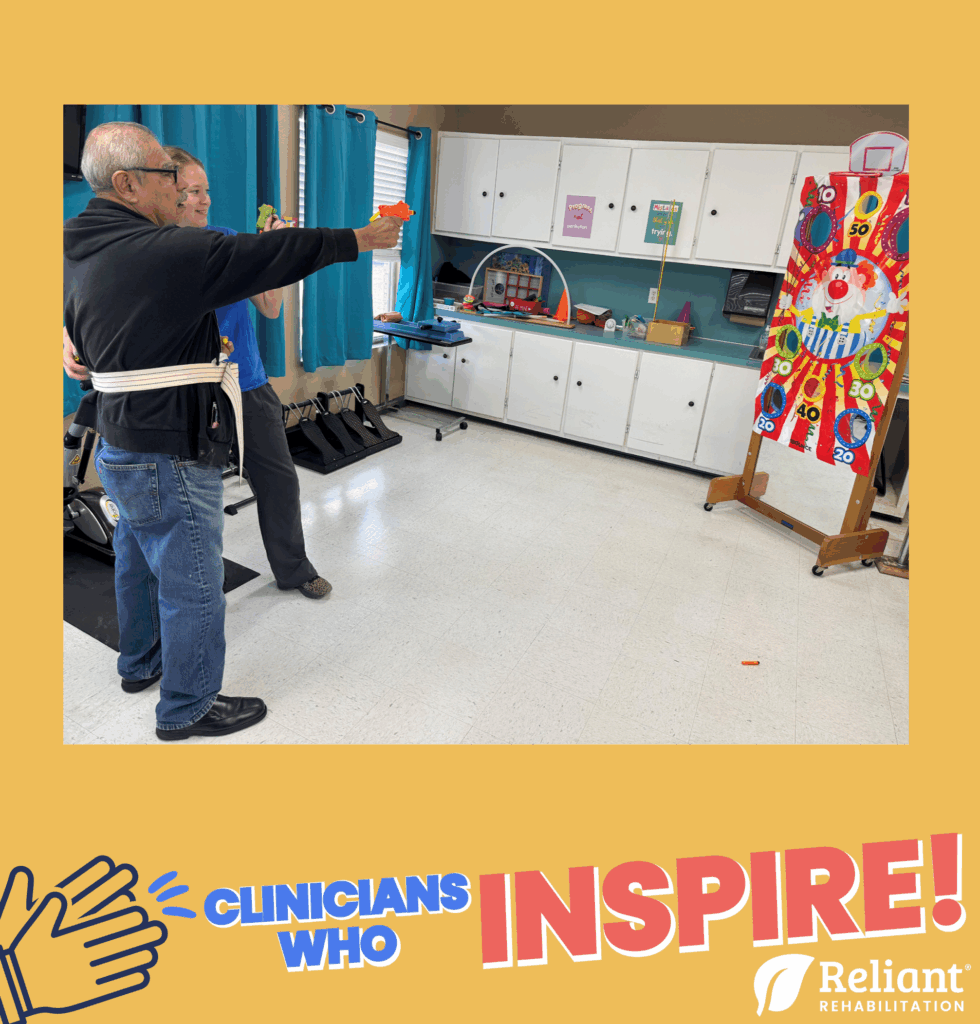
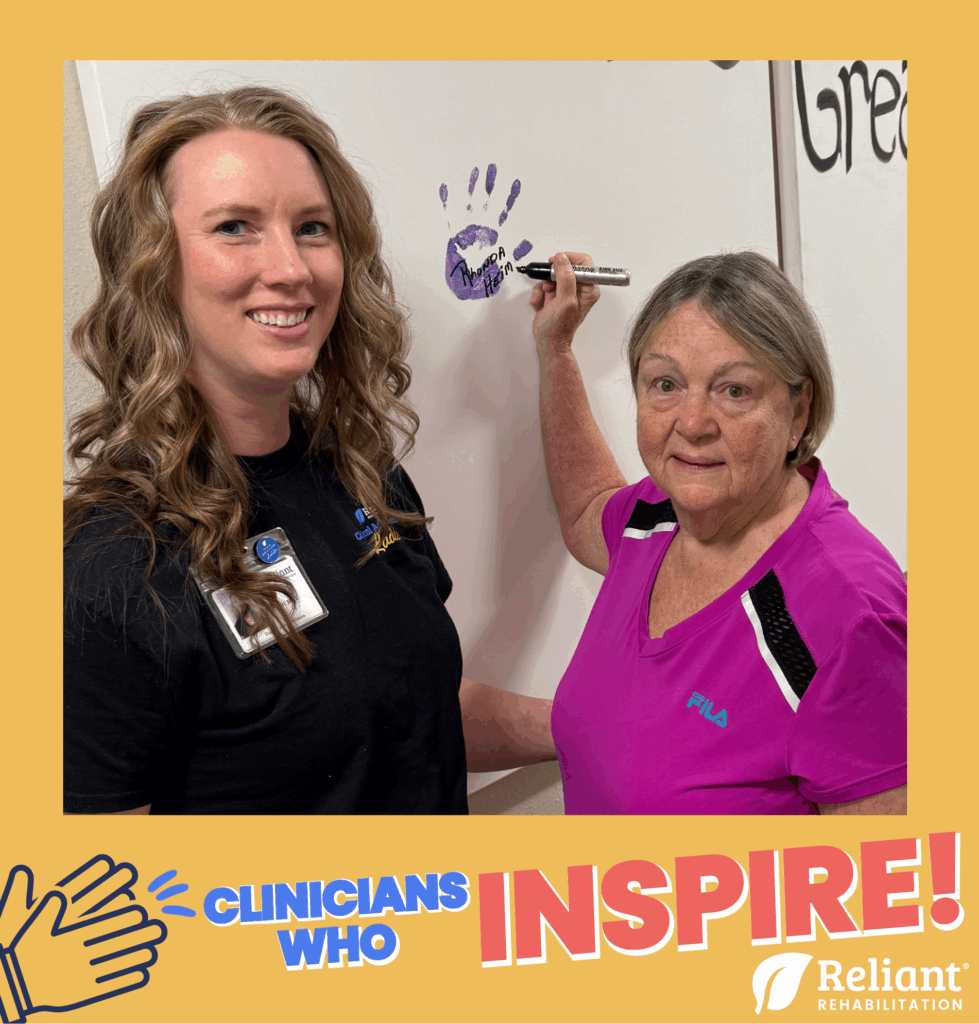
Abby loves to incorporate seasonal activities into therapy interventions. Residents can be seen painting, coloring and constructing gingerbread houses, and decorating the Christmas tree in the gym, all while working on their patient specific goals! To enhance the festive atmosphere, Christmas music or holiday movies are often playing in the background while residents are busy in the gym.
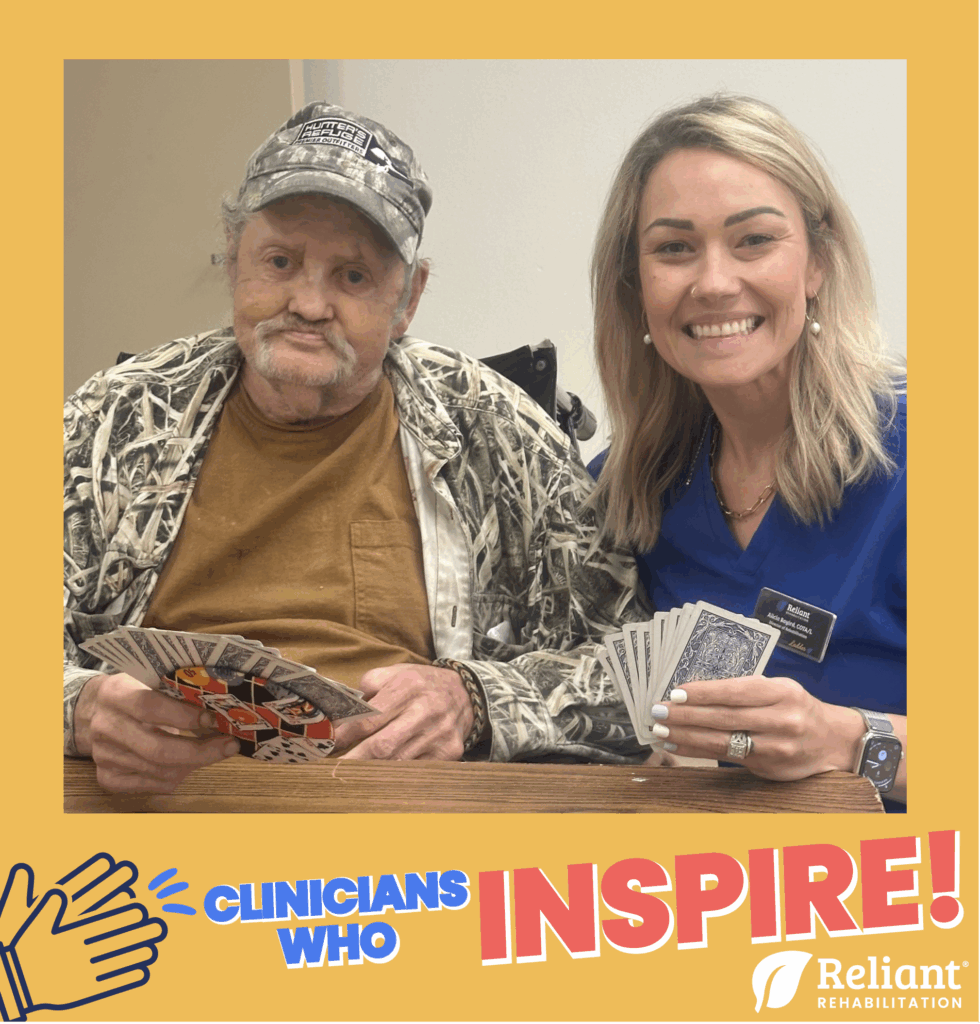
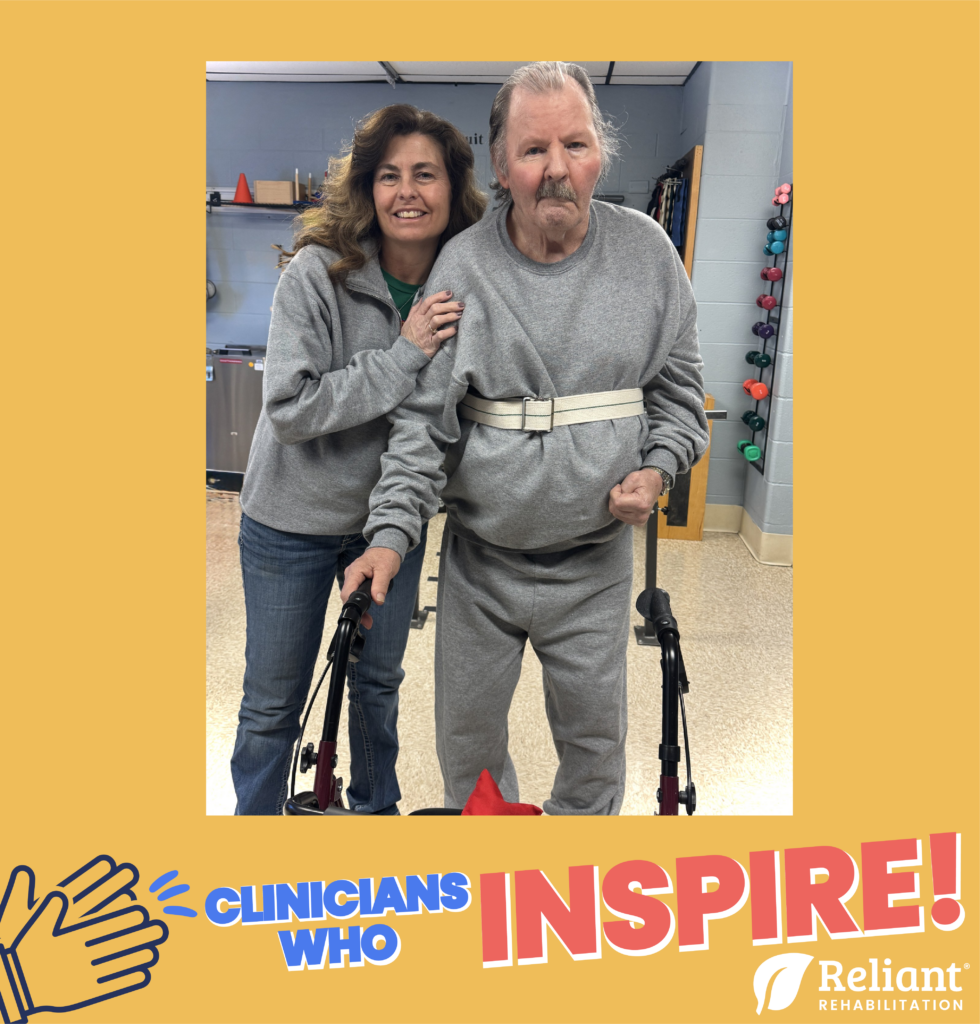
Abby talked of how patience and encouragement are key to keeping a positive gym and therapy environment. She explains that if a resident is taking a nap, she allows them to finish resting and returns later for therapy. If they’re hesitant about participating, Abby educates them on the benefits of therapy and provides positive encouragement. Having music playing in the gym and snacks on standby helps encourage participation in therapy as well. Abby shares that “everyone loves to come to therapy. It’s a positive place.”
Abby leads by example with open communication and ensures everyone in the facility works together for the wellbeing of the patients. Abby, thank you for spreading positivity and being a Clinician Who Inspires!